
Zim Now Writer
Zimbabwe is facing mounting financial strain as it battles to sustain third-line antiretroviral treatment for over 600 individuals living with HIV. The country is currently spending thousands of dollars each month to provide advanced therapy for 603 patients—at a time when global donor support is steadily declining.
The Ministry of Health and Child Care says the growing demand for third-line treatment is becoming unsustainable due to its high cost and the complexity involved in managing patients who have developed resistance to earlier treatment options.
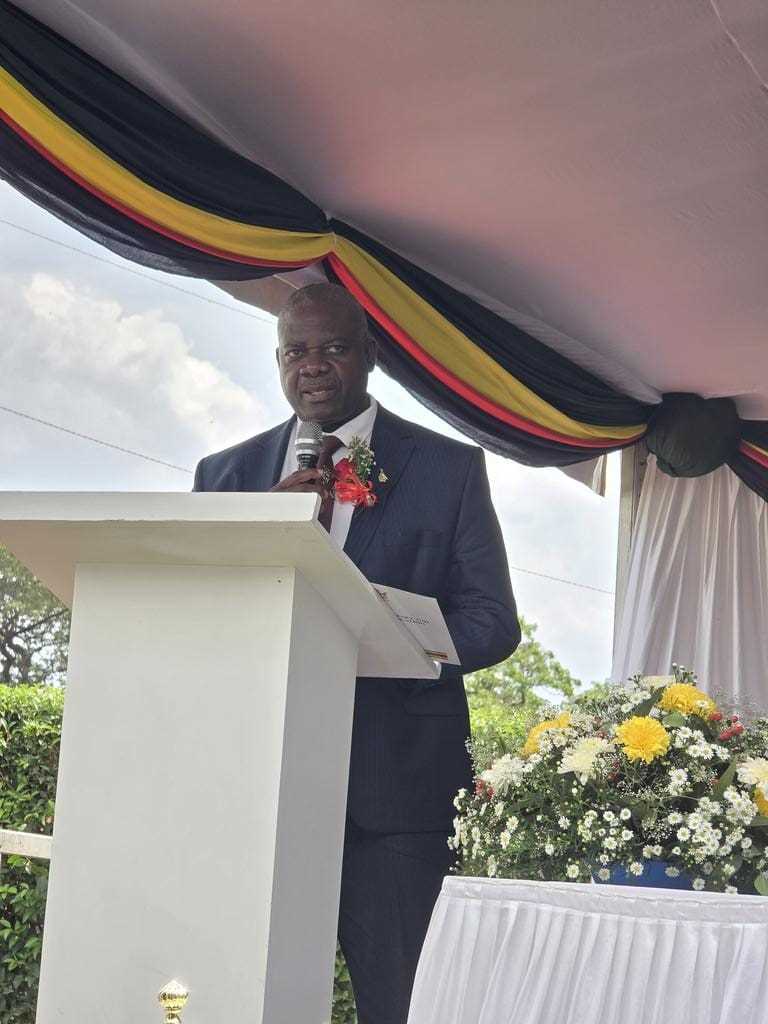
“The challenge with third-line treatment is that it is expensive to manage. First-line costs between US$6 and US$8 per month, while the third line goes into hundreds or even thousands of US dollars per person,” said Dr. Owen Mugurungi, Director of the AIDS and Tuberculosis Unit.
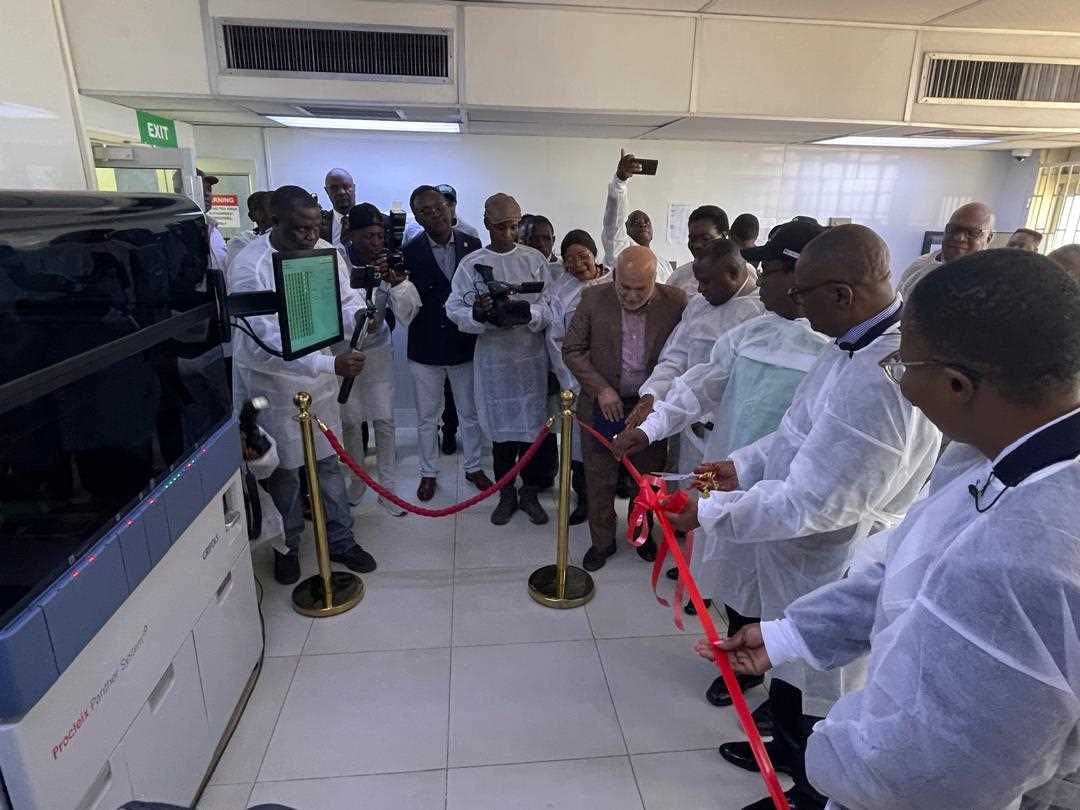
Unlike first-line ARVs, which remain widely available and affordable, third-line regimens require specialized drug resistance and sensitivity testing, which can cost thousands of dollars. These tests are not standardized and must be tailored to each patient’s specific condition.
Adding to the problem is the limited global supply of third-line ARVs. Because of low demand, these drugs are not manufactured in large quantities, making them more expensive and their availability uncertain.
“These drugs are not produced in large quantities due to low demand globally, which makes them extremely expensive and their availability uncertain,” said Dr. Mugurungi.
Related Stories
Health officials attribute the rising need for third-line treatment largely to drug resistance caused by poor adherence to medication. Misinformation from traditional and spiritual healers continues to mislead some patients, resulting in treatment interruption or abandonment.
“Some patients are told by traditional or spiritual healers that their illness is not HIV, leading them to stop taking ARVs. This kind of misinformation is dangerous,” Dr. Mugurungi explained.
He further warned that when patients interrupt treatment—whether due to side effects, stigma, or forgetfulness—the HIV virus can mutate and become resistant to existing medications, making it more difficult and costly to treat. In some cases, individuals are already infected with resistant strains, necessitating immediate third-line intervention.
To improve adherence and ease access, the Ministry is now dispensing ARVs in six-month supplies, with the option for patients to appoint someone else to collect the medication on their behalf.
“This ensures people remain on treatment and don’t run out of medication due to travel or access issues,” said Dr. Mugurungi.
As part of its strategy, the Ministry is also working with the media to debunk harmful myths and promote consistent treatment adherence.
Since the introduction of ARV therapy in 2004, Zimbabwe has made significant progress in its fight against HIV. However, the growing need for advanced treatment is presenting new challenges that threaten the sustainability of its health response.
With donor funding shrinking and treatment costs rising, the government faces a tough balancing act: maintaining access to life-saving medication while ensuring affordability and long-term sustainability.

















Leave Comments