Audrey Galawu- Assistant Editor
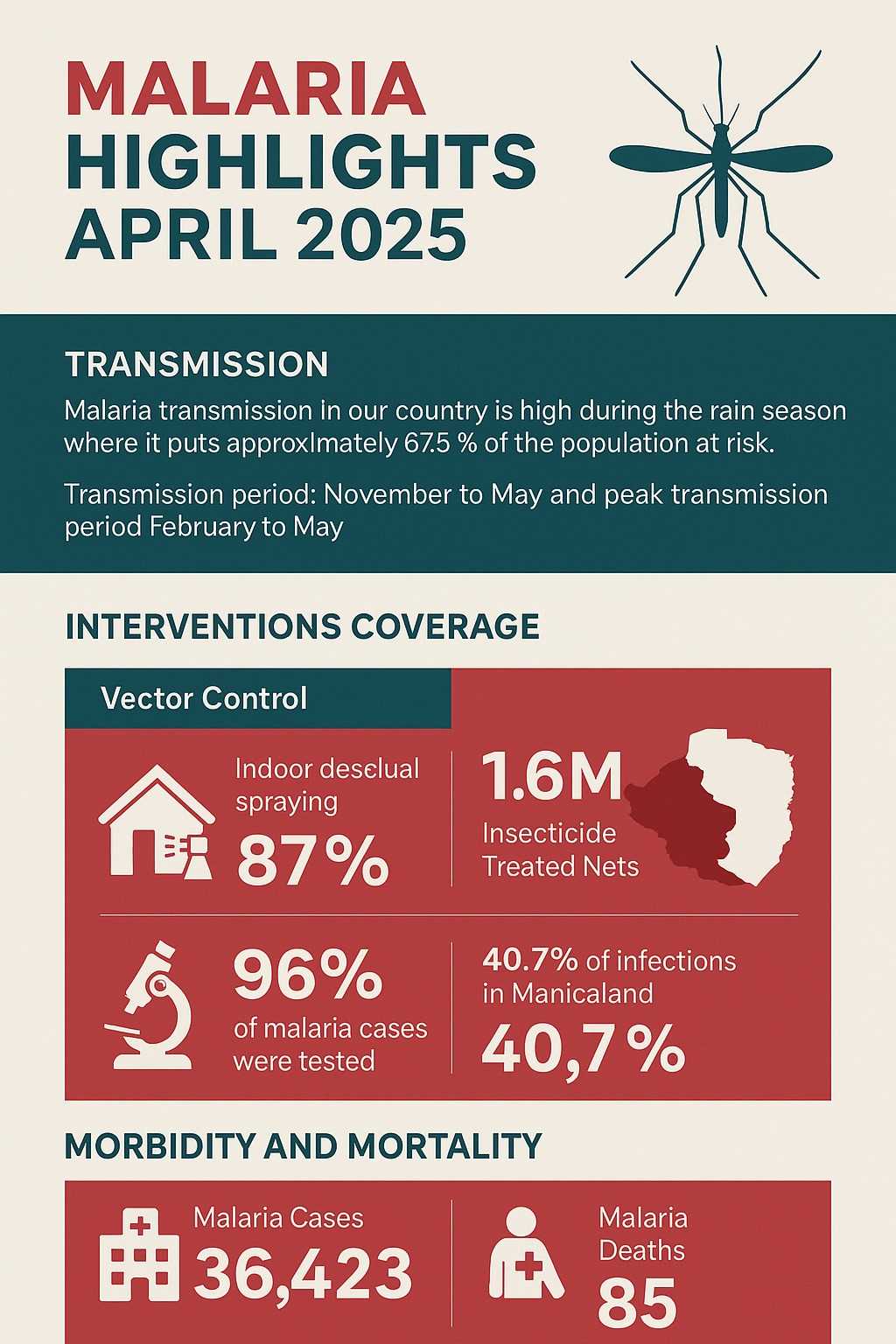
As Zimbabwe enters the peak of its rainy season, malaria transmission has sharply risen, placing approximately 67.5% of the population at risk.
The Ministry of Health and Child Care has reported a significant increase in malaria cases and deaths between January and mid-April 2025, underlining the importance of prevention and prompt treatment.
According to the Ministry’s latest statistics, cumulative malaria cases from Week 1 to 15 of 2025 soared to 36,423 — a 107% increase compared to 17,539 during the same period in 2024. Deaths also rose dramatically, from 21 last year to 85 this year.
Health officials attribute the spike to a combination of climatic conditions – including increased rainfall, humidity, and temperatures – as well as intensified outdoor activities such as farming and artisanal mining.
Manicaland Province remains the hardest hit, accounting for over 40% of reported malaria cases and nearly 39% of all malaria-related deaths. Mashonaland Central followed with 28.2% of cases.
Notably, most of the cases reported in Harare and Bulawayo were either imported or referred for complications to tertiary hospitals. Children under five years old made up 14% of the cases, highlighting the continued vulnerability of young children to the disease.
Related Stories
Despite the surge, Zimbabwe continues to implement robust malaria prevention strategies based on World Health Organization recommendations. These include indoor residual spraying (IRS), distribution of insecticide-treated nets, timely testing and treatment, intermittent preventive treatment for pregnant women, social and behaviour change campaigns, epidemic preparedness and surveillance.
During the 2024/2025 IRS season, all 22 high-burden districts were reached, with 87% of targeted rooms sprayed, protecting over 2.5 million people. In 2024 alone, more than 880,000 ITNs were distributed, and the government is currently distributing an additional 1.6 million nets to 206 wards in 14 districts.
However, a shortfall of 600,000 nets has emerged due to the withdrawal of U.S. Government (USG) funding, prompting the Government of Zimbabwe to explore ways to fill the gap.
In terms of treatment, the country remains well-stocked with malaria medicines and diagnostic kits for 2025. The Ministry emphasizes the importance of seeking treatment within 24 hours of symptoms to avoid progression to severe disease or death.
Common symptoms of malaria include fever, chills, headache, sweating, joint pain, nausea, and fatigue. Severe malaria may present with extreme weakness, jaundice (yellowing of the eyes), dark urine, and an inability to sit or stand.
To reduce the risk of infection, the Ministry advises the public to: Sleep in sprayed houses or under ITNs every night, use mosquito repellents and wear long-sleeved clothing, especially between sunset and sunrise and seek testing and treatment immediately when symptoms appear.
“Malaria is both preventable and curable,” reads a statement from the Ministry, “but it can be deadly if left untreated. Communities must remain vigilant, especially during this high transmission period.”
















Leave Comments