
Bridget Mabande
Even the most radical feminists of today - who are fanatic about the “marriage is no achievement” mantra- may just about forgive Sophia Hamadziripi of Matekaire Village in Chivi, for her excessive jubilation on the marriage of her daughter Mazviona Chivurugwi.
"I am so happy that my daughter got married. With her condition, and stigma from society, it is not something that was expected,” says Sophia.
Mazviona got married to Ian Museve in 2018 and the couple are the proud parents of one baby.
According to Sophia, Mazviona was born with mental illness.
Mental illness is defined a developmental brain disorder with genetic and environmental factors leading to the altered circuits and altered behaviour and it ranges from autism to schizophrenia.
Her husband has a similar condition. With the support of his parents, Ian paid lobola for Mazviona and they have been living together with the support of both families.
Zimbabwe joined the rest of the world to commemorate World Mental Health Day on 10 October.
The World Health Organisation says the overall objective of World Mental Health Day is to raise awareness of mental health issues around the world and to mobilize efforts in support of mental health.
Who also says the Day provides an opportunity for all stakeholders working on mental health issues to talk about their work, and what more needs to be done to make mental health care a reality for people worldwide.
Who estimates that around 450 million people suffer from a mental or behavioural disorder which account for 12% of the total global burden of disease.
Zimbabwe's Ministry of Health and Child Care says there are at least 1.3 million people living with mental illnesses in Zimbabwe.
In a paper titled “The causes of mental illness among Shona people by Shona elders in Harare” by Percy Taruvinga and Victor Moyo explore how mental illness is perceived by society.
They say popular perception attributes congenital mental health problems to witchcraft, substance abuse, generational curses (kutukwa nevadzimu), improper use of love portions (mupfuhwira), stress (kushungurudzika pakufunga) according to a research by drug and alcohol abuse.
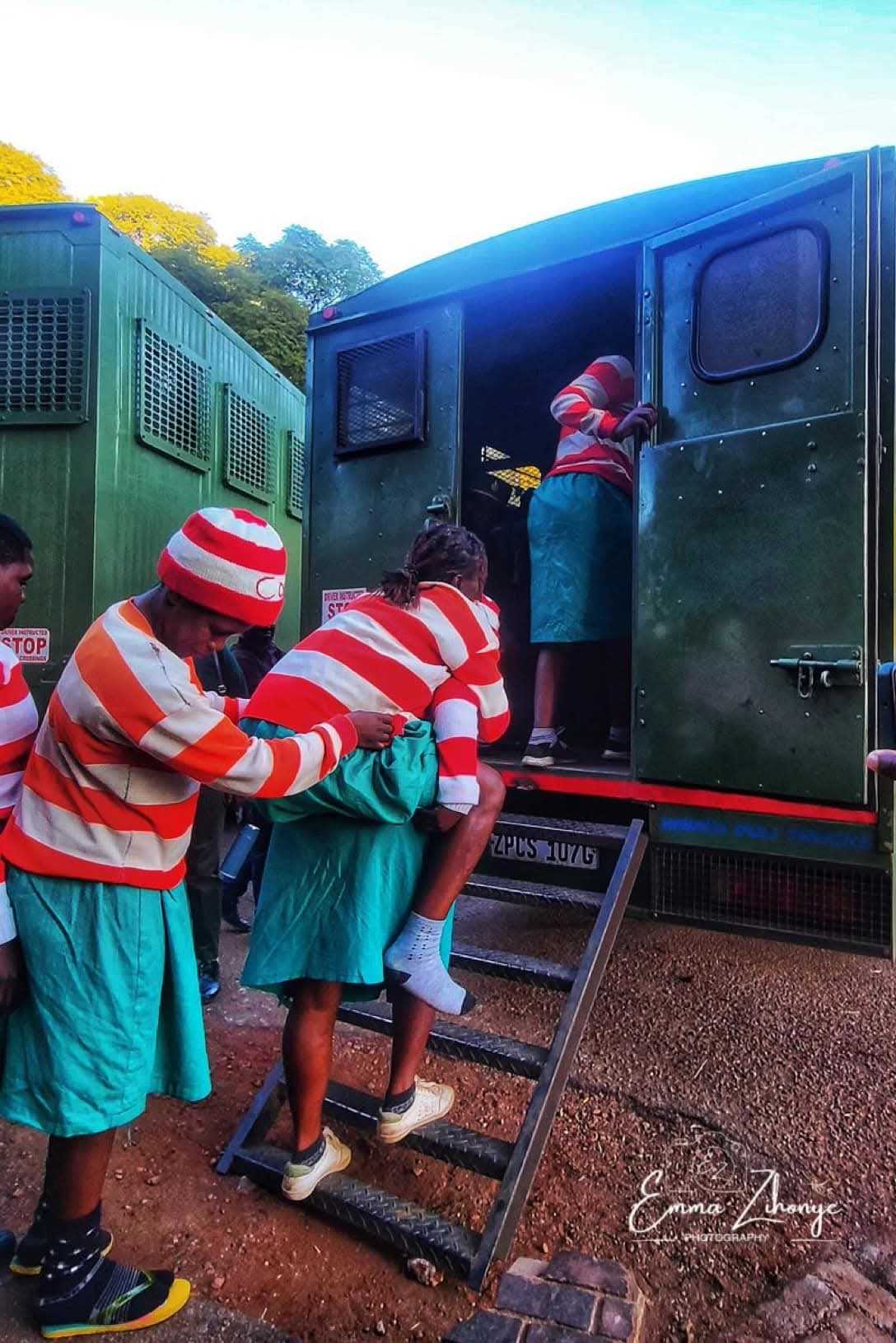
People living with mental illness are often devalued and have to endure hearing hurtful comments, being treated as less competent, being told to lower their expectations in life and being shunned or avoided according to Canadian Mental Health Association.
Mental illness and reproductive health rights
Women with mental illness are often have no choice over their reproductive life. They are either overprotected as they are perceived as children or just relegated to peripheries of society.
Related Stories
When one sees a woman with mental illness pregnant, the assumption is that she is a victim of rape. The law in Zimbabwe does not recognize the right to sex for people with mental health.
Yet if they get support on conversations about sexual choice, safety, preferred method of contraception and family planning as part of routine some people with mental health challenges can make informed choices.
“I encourage people to support their children in what they want to do," said Hamadziripi. By believing in Mazviona as a capable human, Hamadziripi has raised a woman who is independent and self-sufficient, rising above the supposed boundaries of her mental illness.
Mazviona is currently employed as domestic worker in Zvishavane while Ian lives at home in Museve Village in Chivi.
Research show that women’s mental health cannot be achieved without equal access to basic human rights: autonomy of the persons, education, safety, economic security, property and legal rights, employment, physical health including sexual and reproductive rights, access to health care and adequate food, water and shelter.
Johnson Chivurugwi, who has a sister diagnosed mental illness wants a shift from urban mental services to community health services.
"General practitioners and mental health clinicians require training in the skills to talk to women about their sexual and reproductive health and to support women to make choices that protect this alongside their mental health needs," said Chivurugwi.
His sister, Esther got pregnant last year and could not name the man responsible.
Chivurugwi said there should be enhanced access to sexual and reproductive health services for women with mental illness as they are a key population.
"These people are more likely to experience increased risk of sexually transmitted infections, gynaecological diseases and reproductive health cancers. Then of course the pregnancies.
"People like Essie need to be given birth control pills or other forms of contraception because any man can take advantage of them," said Chivurugwi. Essie’s family now has the responsibility of looking after her as well as the child of unknown paternity.
Online search shows around 20 registered clinical psychologists and nine mental health institutions for a country with a population of 15 million. This shows that access to necessary medical service for diagnosis, treatment and management is severely limited.
Those like Essie, who live in marginalized areas are therefore even more vulnerable.
There is increasing evidence that midwife‐led continuity of carer systems improves pregnancy and infant outcomes among at-risk groups.
Such models should be extended to include specific programming for women with mental health illnesses.
With a qualified person who understands their specifc sexual and reproductive health needs, these women can have control over their reproductive health.

















Leave Comments