Audrey Galawu
Assistant Editor
Imagine a world where common infections become untreatable, surgeries too risky to perform, and basic health care collapses under the weight of drug-resistant diseases.
This is not a distant dystopia but an imminent reality, driven by the growing crisis of antimicrobial resistance.
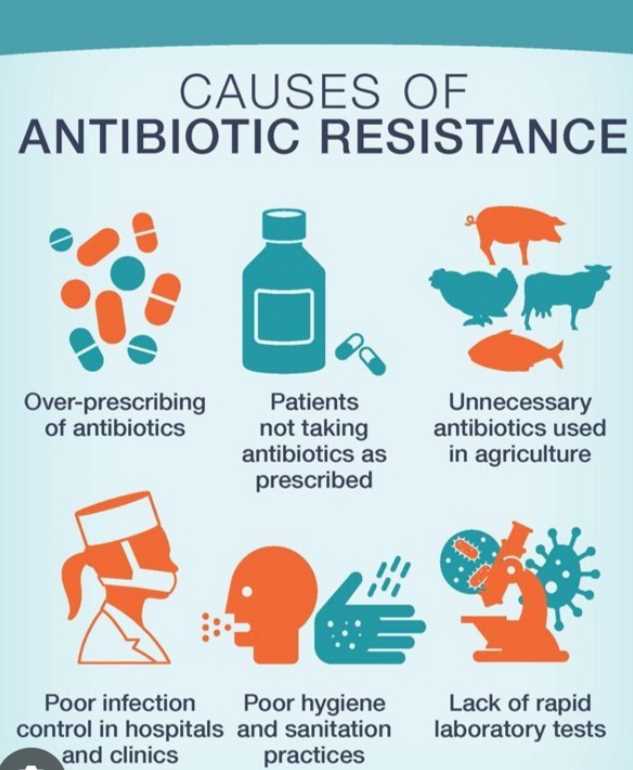
AMR, often called the "silent pandemic," happens when microorganisms such as bacteria, viruses, fungi, and parasites develop resistance to medicines.
This renders treatments ineffective, transforming minor ailments into life-threatening conditions.
Wrong diagnosis and inappropriate prescriptionby medical professionals is a factor in AMR.
Felix Liauw from Indonesia watched his three-month-old son die after being diagnosed incorrectly with sepsis.
The baby endured escalating antibiotic treatments before a genetic test revealed the real issue: congenital short bowel syndrome.
Instead of being treated for his inability to digest any milk, the boy was given more and more antibiotics.
“We must only use antibiotics or antimicrobials when there is a proper diagnosis,” Felix, now an advocate for the World Health Organisation Task Force of AMR Survivors, urges. “Improper use of these medicines leads to more lives lost.”
Related Stories
AMR's reach extends far beyond hospitals and clinics. In agriculture, resistant pathogens compromise livestock health and productivity, threatening food security for millions. According to the Food and Agriculture Organization, resistant microorganisms can contaminate the food supply chain, spreading diseases that are harder to treat in humans.
Environmental pollution further exacerbates AMR. Wastewater from hospitals, pharmaceutical manufacturing, and agricultural runoff creates ideal conditions for resistant pathogens to thrive. “The environment plays a critical role in the development and spread of AMR,” warns Wondwosen Kibret of the United Nations Environment Programme.
Zimbabwe and other Africans are looming close to crisis with each day as unregulated antibiotics are being sold everywhere with people self diagnosing and self medicating.
Health professionals have repeatedly highlighted that misuse and abuse of antibiotics excerbate AMR risk.
In 2019, AMR directly caused 1.27 million deaths and was a contributing factor in nearly 5 million more. By 2050, it could cost the global economy US$159 billion annually in healthcare expenses, with livestock production in low-income countries projected to decline by 11%.
Recognising the interconnectedness of human, animal, and environmental health, experts advocate for a "One Health" strategy. This approach emphasizes collaboration across sectors to combat AMR holistically.
Global leaders have pledged to reduce AMR-related deaths by 10% by 2030 and ensure universal access to proper infection prevention measures, such as clean water, sanitation, and adequate hygiene in healthcare settings.
Young people are emerging as powerful voices in the fight against AMR. Augusto Baron, of the Quadripartite Youth Engagement Working Group, highlights their role as catalysts for change. “Youth engagement is critical to advancing global commitments and inspiring action,” he says.
AMR poses one of the greatest threats to public health, food security, and economic stability. Yet, the tools to fight it are within reach. Stricter regulations on antimicrobial use, investments in diagnostic tools, public education, and global cooperation are essential.
World Antimicrobial Resistance Awareness Week (18-24 November) is a stark reminder that AMR is not just a health issue—it’s a global emergency. Addressing it requires the collective effort of governments, industries, and individuals.
The time to act is now, before the hidden enemy becomes an unstoppable force.

















Leave Comments