
Munyaradzi Doma
Infections caused by bacterial antimicrobial resistance led to the death of 1,27 million people globally, a recent 2nd Annual Global Media Forum webinar on World Antimicrobial Awareness revealed.
Webinar were told that according to the 2019 study which is the most comprehensive to date, almost 5 million deaths were associated with bacterial AMR.
Speaking during the webinar, Thomas Joseph, Head of Antimicrobial Stewardship and Awareness Unit at World Health Organisation (WHO) said “lower respiratory tract infections like pneumonia, accounted for more than 1.5 million deaths associated with AMR in 2019, making it the most burdensome infectious syndrome of our time.”
AMR occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines, making infections harder to treat and increasing the risk of disease spread, severe illness and death.
As a result of the drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat.
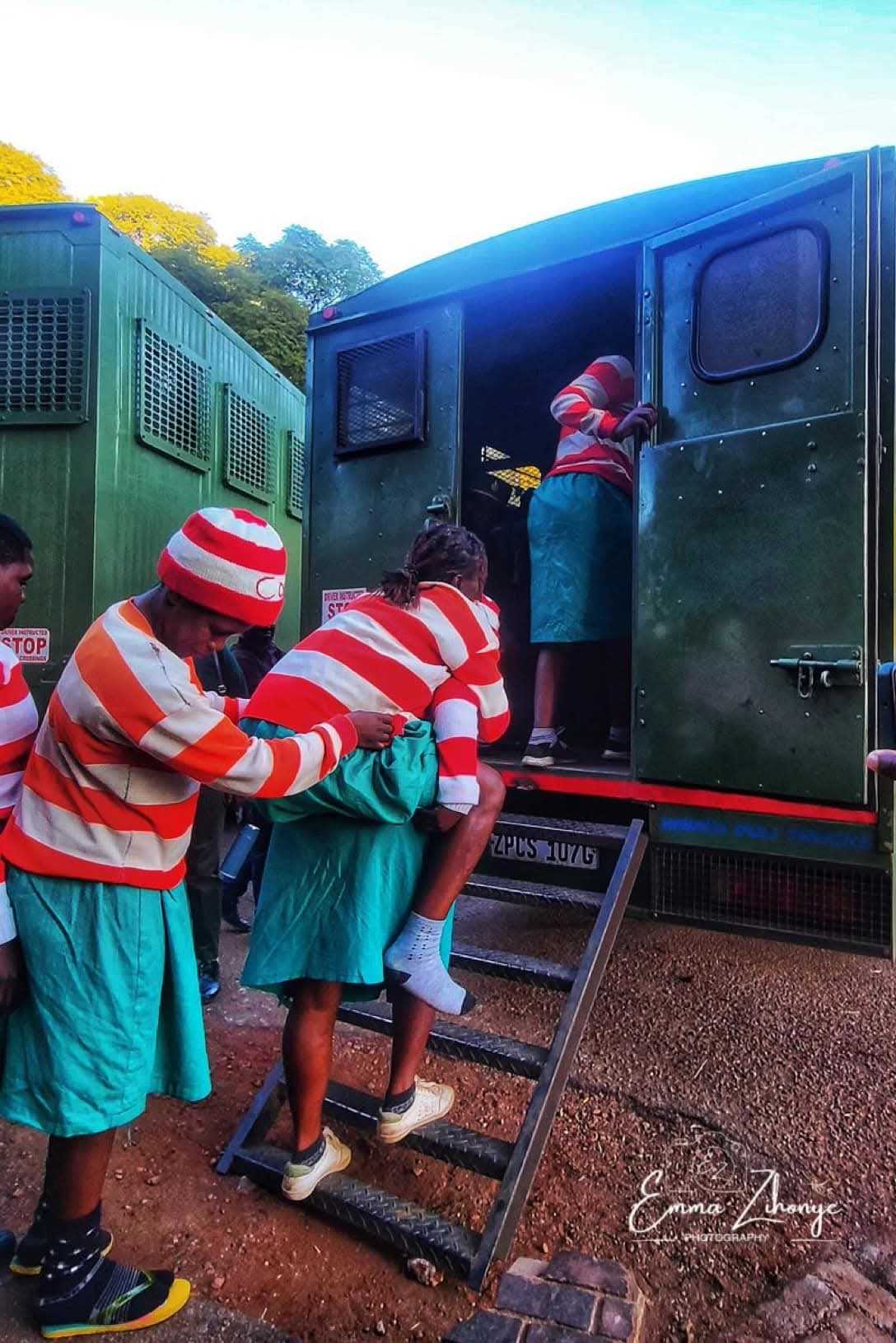
Zimbabwe has the problem of antibiotics being sold illegally on the streets, meaning that many people are now self-diagnosing and self-treating. This is likely to result in overuse, misuse and improper administration of antibiotics. These are all factors that can drive AMR, according to experts.
“The burden of antimicrobial resistance is greatest in low-resource settings, particularly sub-Saharan Africa, and South Asia, which already carries much of the world's burden of communicable diseases.
“AMR is therefore not only a global public health problem, but also an issue of health equity and socioeconomic development.
“Drug resistance also affects medicines used in treatment of fungal, and parasitic infections, such as HIV and malaria besides TB.
Related Stories
“A person with a drug-resistant infection is more likely to be sick and absent from work and family commitments, for longer, and require more expensive medicines and medical care.
“This has major implications on health-care costs and productivity, both for patients and their caregivers, as well as more broadly on the health system and national economy,” revealed Joseph.
He said drug-resistant infections often require the use of second- or third-line treatments, which are usually more expensive, not widely available and can cause serious side-effects like organ failure.
Joseph said that AMR was being worsened because of the misuse and overuse of antimicrobials to treat or prevent infections in humans, animals, and plants.
“If antibiotics and other antimicrobials lose their effectiveness, we lose the ability not only to treat infections, but also to manage these other health conditions.
“Antibiotics are lifesaving, but they should only be taken when they have been prescribed by a health worker for bacterial infections.
“Unnecessary exposure to antibiotics, such as when they are prescribed and used for conditions that are not caused by bacteria, like colds and flus, allows antibiotic-resistant strains to develop.
“Not all people with common infections in the community should routinely receive antibiotics. In many cases infections may be caused by viruses, which do not respond to antibiotics.
“Each year hundreds of millions of cases of diarrhoea in humans are treated with antimicrobials. Universal access to clean water, sanitation and hygiene could reduce this by 60%,” added Joseph.
He added that while people rush to treat bacterial infections, more should also be done to ensure prevention by practicing good hygiene.
He reiterated that prevention measures reduce the likelihood of infection hence antibiotics will not be needed.


















Leave Comments