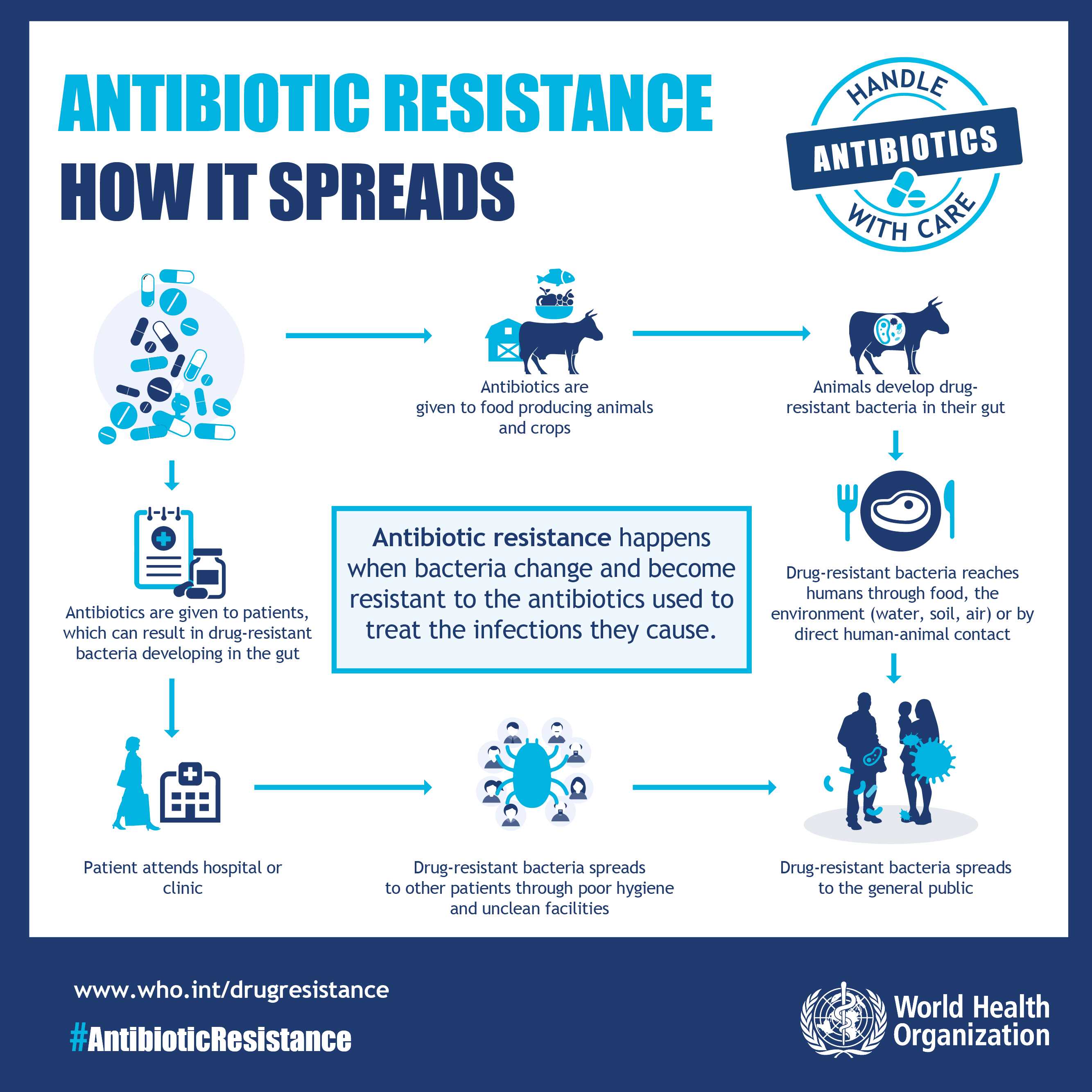
Antimicrobial resistance the ability of microbes to withstand the drugs designed to kill them — is emerging as one of the most serious threats to global health, economies and food systems in this decade and beyond.
At the 2025 World Economic Forum in Davos, global leaders, private sector partners and health experts launched the Davos Compact on AMR, pledging unprecedented collaboration to prevent a future where antibiotics and other life‑saving treatments fail.
“Our goal is simple: to unlock sustainable and synergistic financing from both public and private sources to reduce the global deaths associated with AMR, saving more than 100 million lives by 2050,” the Compact declares. This marks a shift from political statements to finance‑backed action, bringing governments, philanthropies and businesses together in what leaders call the Unified Coalition for the AMR Response.
A Crisis Measured in Millions
AMR is already a major killer. According to global estimates, more than 4.7 million people died in 2021 in association with drug‑resistant infections, including 1.14 million deaths directly attributable to resistance.
If nothing changes, the threat will only grow: between 2025 and 2050 more than 39 million people could die directly from AMR, with a broader 169 million deaths linked to drug resistance in that period.
The World Health Organisation has also reported that one in six bacterial infections worldwide is now resistant to standard treatment, a figure driven by decades of misuse, overuse and weak surveillance systems — particularly in low‑ and middle‑income countries.
The Davos Compact lays out four key pillars for action:
Innovation and Access: speeding up research and development of new antimicrobials, diagnostics and vaccines, while ensuring equitable access.
Awareness and Advocacy: elevating understanding among policymakers, health workers and the public about AMR risks and prevention.
Sustainable Agri‑Food Systems: reducing unnecessary antimicrobial use in livestock and crops, and promoting better stewardship, biosecurity and husbandry.
Multisectoral Engagement and Funding: mobilising public, private and philanthropic capital to scale up AMR solutions globally.
The Compact underscores the need for “One Health” action — recognising that human, animal and environmental health are interconnected in the evolution and spread of resistance.
In sub‑Saharan Africa, AMR’s toll is already serious. A WHO brief has noted thousands of direct AMR deaths each year, with resistance complicating treatment of common infections and straining already fragile health systems.
Related Stories
In Southern Africa specifically, resistance rates often exceed 70% for some key bacterial strains, especially those causing bloodstream and urinary infections — making effective treatment progressively harder.
In Zimbabwe, surveillance projects reveal a worrying trend. Resistance to standard antibiotics is prevalent, with a drug resistance index above 60 percent, implying that more than half of common infections are no longer reliably treatable with first‑line drugs. This means clinicians increasingly must rely on second‑ or third‑tier medicines that are more expensive, less available and often harder on patients.
Public awareness remains low: in some community surveys, fewer than 20 percent of rural Zimbabweans could accurately define antimicrobial resistance or link it to antibiotic misuse, a gap that health advocates say must be closed urgently.
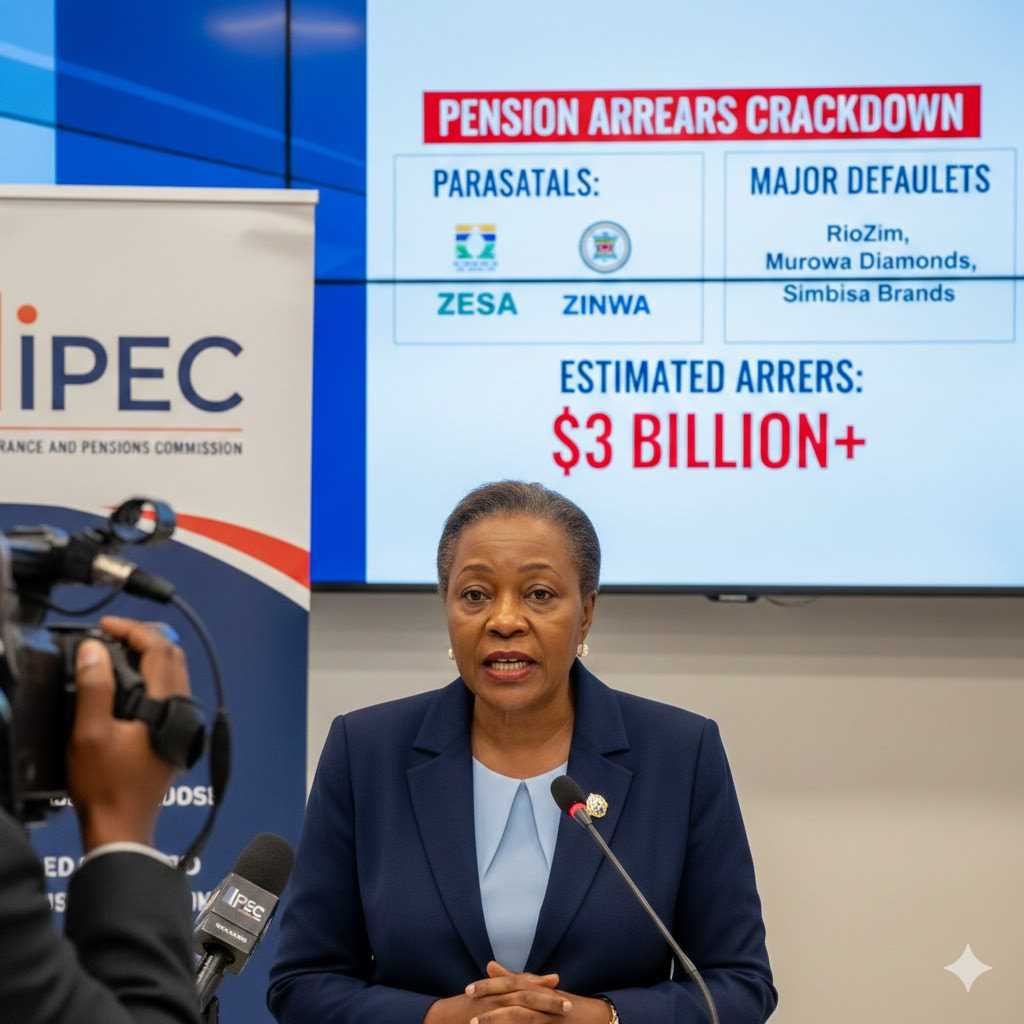
AMR isn’t only a health crisis — it’s an economic one. The World Bank has warned that if left unchecked, resistance could reduce global GDP by about 3.8 percent annually by 2050, pushing millions into poverty as treatment costs rise and productivity falls.
AMR also erodes gains in food security. Resistant infections in livestock reduce productivity and increase feed and treatment costs, while resistant pathogens can spread from animals to humans through food, water and the environment — exactly the cycle the Davos Compact’s sustainable agri‑food pillar aims to disrupt.
Public health specialists stress that Africa’s weakest surveillance systems and frequent over‑the‑counter availability of antibiotics heighten risk. In many rural clinics, bacterial infections are treated empirically without laboratory data, accelerating resistance.
“In Zimbabwe and across Southern Africa, every unnecessary antibiotic prescription chips away at our ability to treat real infections,” said a regional infectious disease specialist. “We need not only new drugs, but also better diagnostics, stewardship and community education.” (Expert testimony paraphrased from global health sources)
Turning Commitments Into Action
The Davos Compact sends a clear message to policymakers: political will alone isn’t enough. Sustainable financing, private sector engagement, and measurable country‑level action are now required.
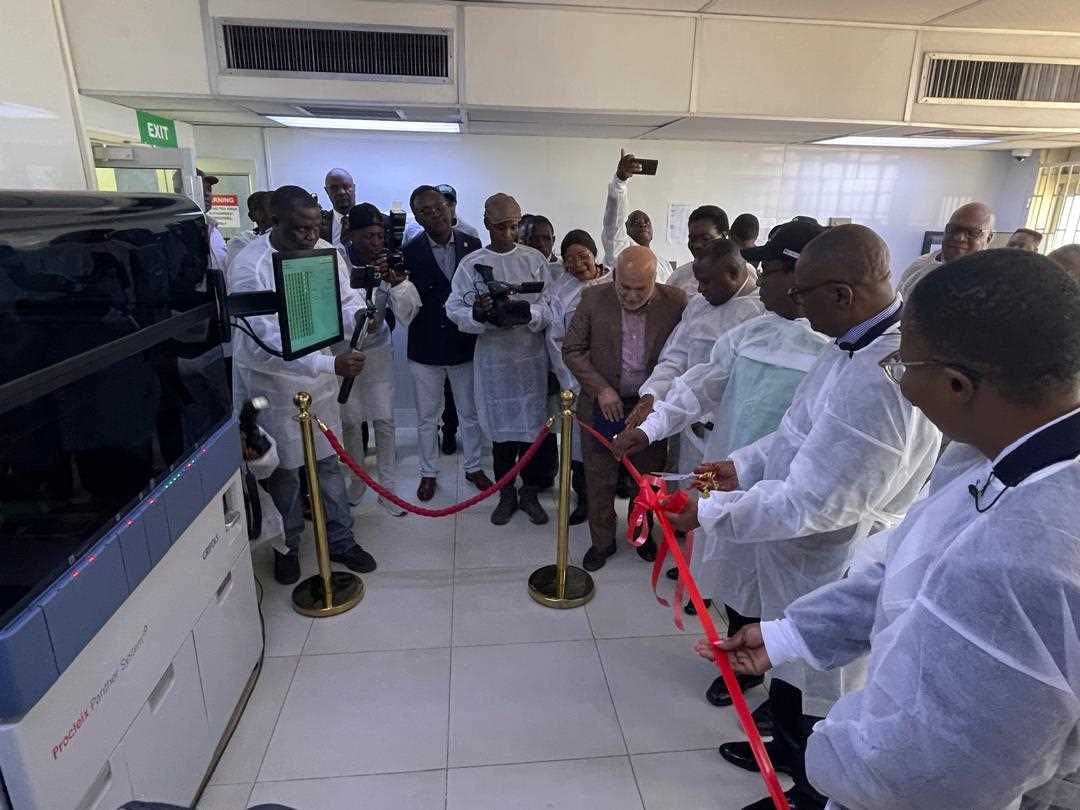
For Zimbabwe, this means aligning national AMR strategy with global frameworks such as UCARE, investing in laboratory capacity, strengthening regulation of antibiotic sales, and embedding AMR education into community health programmes.
For the region, collaborative networks — sharing surveillance data, harmonising regulatory policies and training health workers — could slow the tide of resistance and save lives.
“The science is undeniable,” global health leaders warned at Davos. “If we act now, we can avert millions of deaths — but delay increases human suffering and economic loss.”
The Costs of Inaction
Without decisive action, AMR could reverse decades of health progress. Routine surgeries, childbirth, cancer treatments and chronic disease management all depend on effective antimicrobials. Every loss of efficacy edges health systems closer to an era where minor infections spiral into fatal illnesses.
But there is opportunity in action: tens of millions of lives could be saved by 2050 with coordinated investment, better access to medicines, strengthened health systems and strategic partnerships that the Davos Compact seeks to ignite.
.

















Leave Comments