Audrey Galawu- Assistant Editor
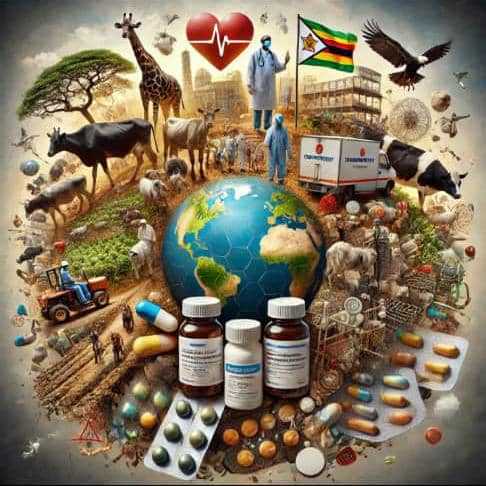
The silent spread of substandard and falsified medicines is worsening the global health crisis of antimicrobial resistance, with low- and middle-income countries, including Zimbabwe, particularly vulnerable.
A World Health Organization report warns that one in ten medical products circulating in these regions fails to meet quality standards, exposing millions to ineffective treatments and accelerating the rise of drug-resistant infections.
“Substandard and falsified medicines cost LMICs more than US$30 billion every year,” said Dr. Philip Mathew, Technical Officer in WHO’s AMR Awareness and Advocacy team.
“Worse still, these poor-quality drugs contribute to between 70,000 and 170,000 child deaths annually, especially due to ineffective antibiotics used for pneumonia.”
In Zimbabwe and across the continent, the availability of fake and poorly manufactured medicines has deadly consequences.
Weak regulatory systems, limited resources, and the high cost of healthcare force many patients to turn to unlicensed markets where these medicines are readily available.
Leena Menghaney, a lawyer and global health advocate, highlighted how access gaps leave patients vulnerable. “People living with advanced HIV, for example, are dying not just from infections like cryptococcal meningitis, but from infections resistant to standard treatments,” she said.
Antimicrobial resistance is now recognised among the top ten global public health threats. Misuse of antibiotics in both human medicine and agriculture plays a major role. “Globally, about 60% of antimicrobials are used in livestock and poultry, with resistant bacteria like E. coli and Salmonella easily transmitted to humans through the food chain,” explained Dr. Kamini Walia, senior scientist at India’s Council of Medical Research and Chairperson of the Global AMR Media Alliance.
Dr. Walia warned that if left unchecked, AMR could kill up to 10 million people a year by 2050, with Africa bearing the brunt, and cost the global economy US$100 trillion.
Closer to home, the Medicines Control Authority of Zimbabwe has made efforts to strengthen surveillance and crack down on counterfeit medicines.
However, underfunded health systems and rising out-of-pocket medical expenses still drive many Zimbabweans to informal pharmacies, where regulation is minimal.
Related Stories
“Medicines containing low or incorrect doses of active ingredients often fail to cure infections,” Dr. Mathew explained.
“This leaves behind the strongest, most resistant bacteria, making future treatments ineffective.”
A WHO report released last year showed a sharp rise in cases of falsified and substandard medicines, with a 36% increase in reported cases from 2017 to 2021. Essential drugs, including antibiotics, vaccines, and even cancer treatments, are frequently compromised.
Public engagement has proven critical in detecting poor-quality medicines. Menghaney shared an example from India where people living with HIV flagged an issue with bitter and crumbling ART pills in early 2024.
“Their alert led to immediate investigation, product recall, and reformulation,” she said. Similar community vigilance could play a vital role in Zimbabwe’s fight against unsafe medicines.
She further argued for more stringent procurement processes that require manufacturers to prove their medicines are bioequivalent and stable under local storage conditions. “Even older, essential medicines like penicillin are sometimes missing from public health programmes because the procurement process lacks such safeguards,” she noted.
To address the crisis, WHO and partners are investing in technology and innovation. One such effort is The Trinity Challenge, which has committed GBP 1 million towards solutions focused on detecting falsified medicines in the Global South.
In a significant step forward in the fight against AMR, Hon. Dr. David T. Mombeshora, the Minister of Health and Child Care, officially launched the Zimbabwe One Health Antimicrobial Resistance National Action Plan 2.0 (2024-2028).
The National Action Plan 2.0 is an ambitious framework built on the One Health approach, recognizing the interconnectedness of human, animal, and environmental health. It sets out five core pillars: raising awareness about AMR risks, strengthening surveillance systems, promoting prevention practices, optimizing the use of antimicrobials, and fostering research and innovation.
Notable among the updates in the new plan is a stronger governance framework, which includes the appointment of an AMR focal point for the environment sector and the decentralization of laboratory information systems to enhance data flow. In addition, the plan expands surveillance to include plant health and fish farming, ensuring all sectors contribute to the collective effort against AMR.
Experts agree that tackling AMR and counterfeit medicines requires coordinated action—stronger regulatory frameworks, cross-border collaboration, local capacity building, and public awareness.



















Leave Comments