
The Asia-Pacific Regional Conference on Antimicrobial Resistance 2025 opened with a stark warning that drug resistance is one of the world’s most pressing health challenges.
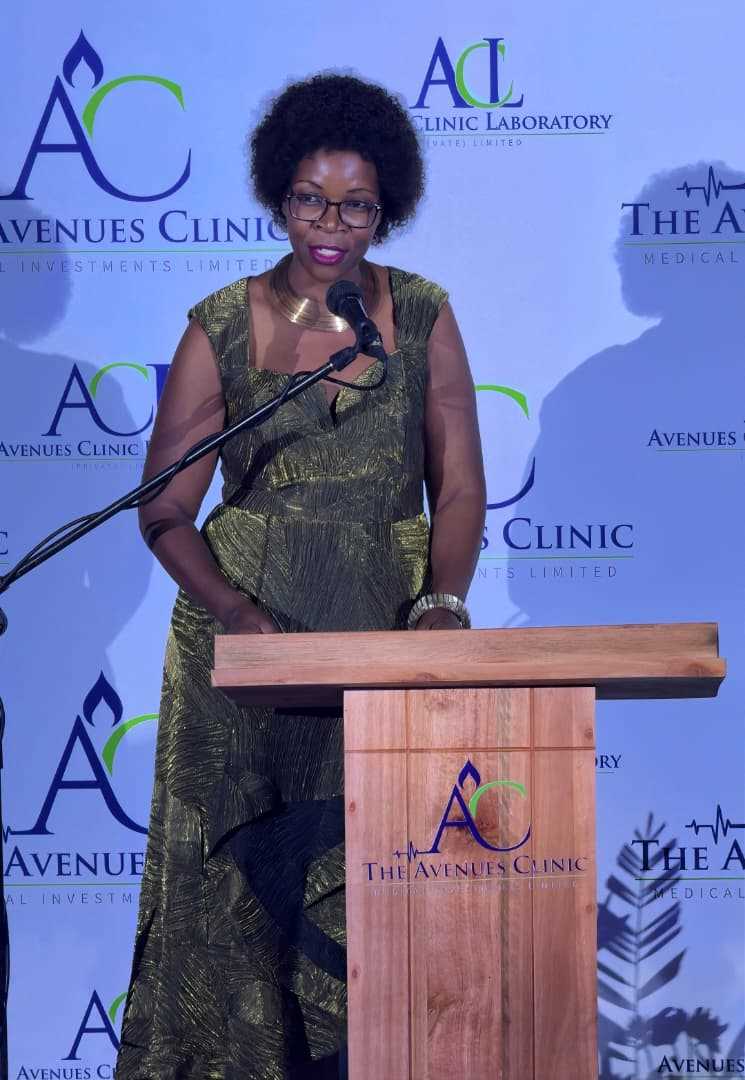
“Antimicrobial resistance is among the top 10 global health threats,” said Shobha Shukla, Chairperson of the Global AMR Media Alliance and recipient of the AMR and One Health Emergent Leaders and Outstanding Talents Award 2024.
Dr SS Lal, Director of ReAct Asia Pacific, stressed the urgency: “It is estimated that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths worldwide.
Asia Pacific region is home to half of world’s population as well as half of global AMR burden.
The misuse and overuse of antimicrobials in humans, animals and plants are the main drivers in the development of drug-resistant pathogens.”
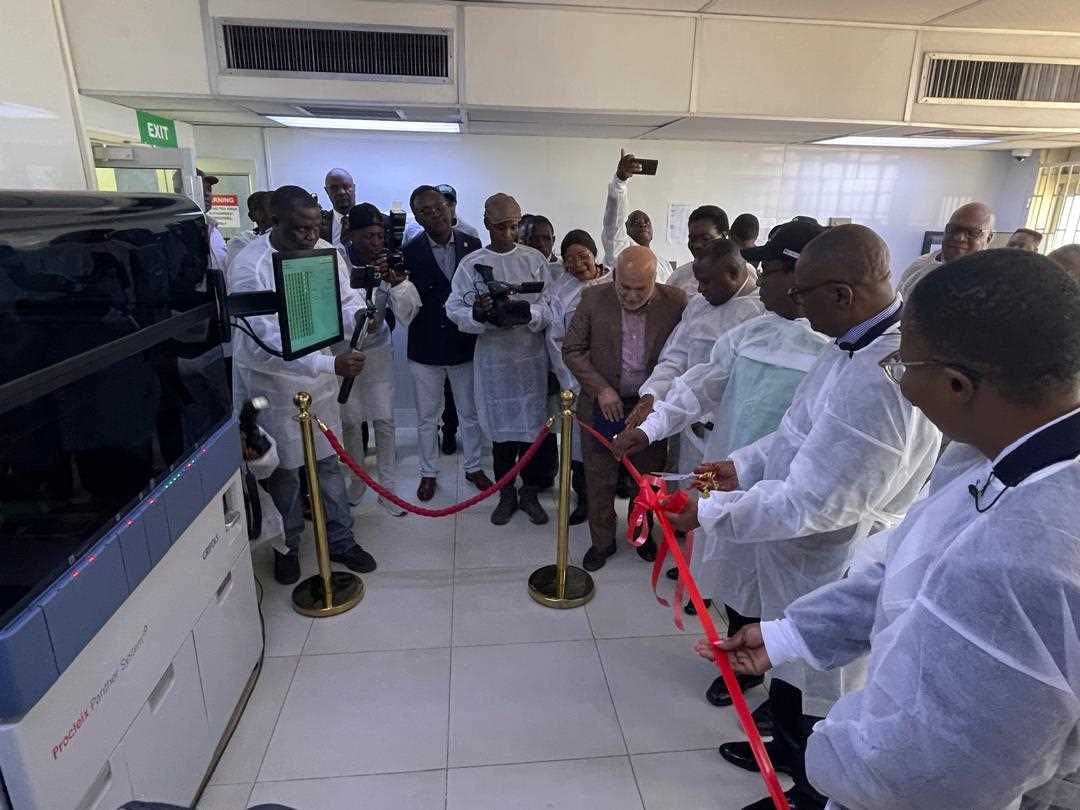
Focus on Diagnostics and Stewardship
Shukla emphasised the role of early and accurate testing:
“If we ensure that right diagnosis – early and accurate diagnosis for all diseases is made possible in rights-based manner for everyone – where no one is left behind – then right diagnosis would become the entry pathway towards right treatment – and stopping misuse and overuse of medicines.
"Infection prevention and control at all levels is so important – and so is multisectoral response.”
Indonesia’s Ministry of Health showcased its leadership, with Dr Amy Rahmadanti highlighting efforts to build hospital diagnostic capacity, procure machines for sentinel hospitals, and develop a referral diagnostic network.
Beyond Global Frameworks
While many countries have national AMR action plans, implementation often falls short.
Related Stories
“Some countries have action plans on AMR but only on paper – without optimal implementation.
"When actions plans on AMR are implemented at national as well as sub-national level, we see many gaps,” said Dr Lal, urging governments to bring civil society, youth and communities into the response.
Anna Sjöblom, Director of ReAct Europe, echoed this point, noting: “Healthy populations will have fewer infections and need for antimicrobials is lesser,” underscoring the value of vaccination, water, sanitation and hygiene alongside stewardship.
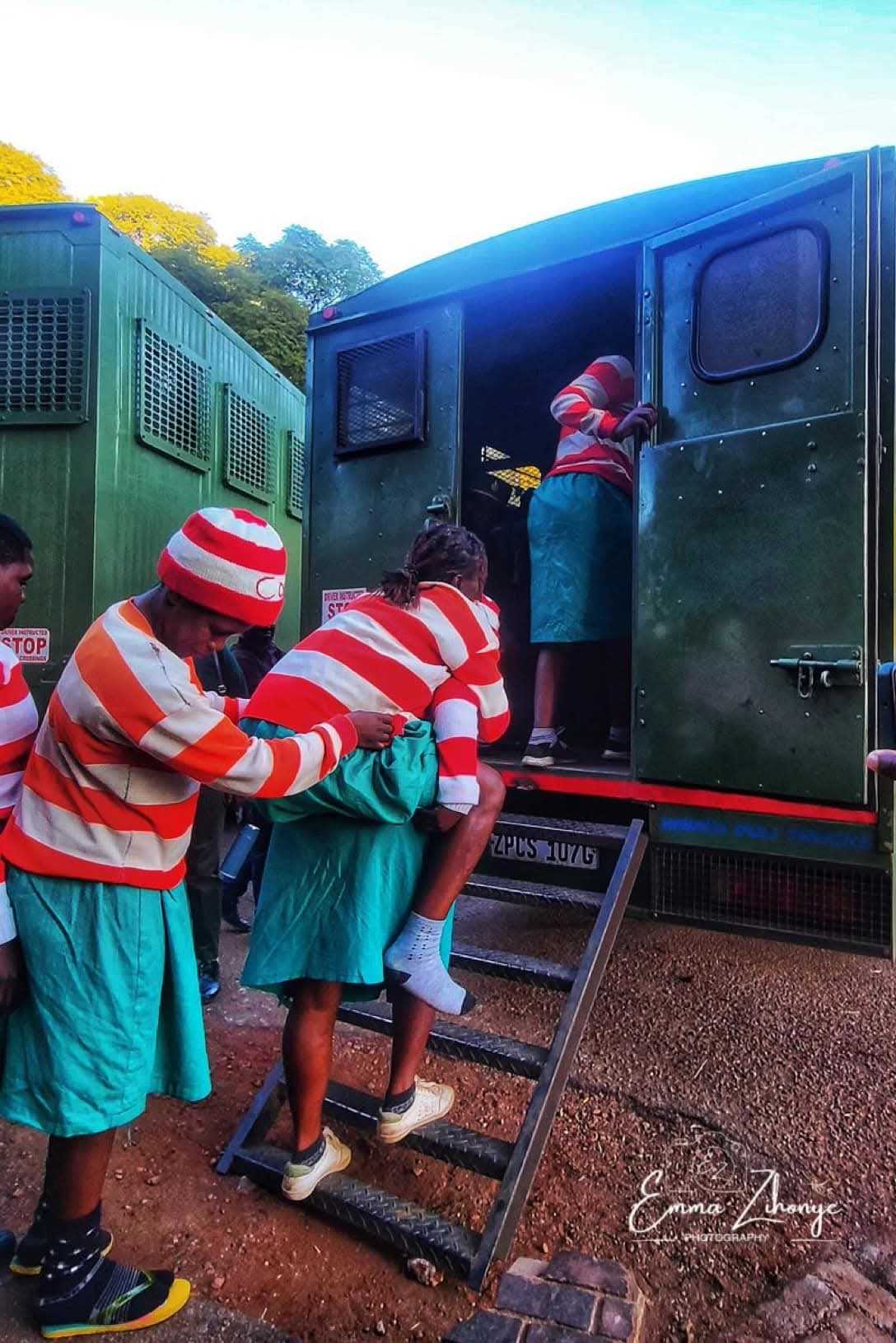
Although the conference focused on Asia-Pacific, African experiences such as Zimbabwe’s underline the scale of the challenge.
- A 2016-2018 analysis found resistance rates of up to 54% among third-generation cephalosporin-resistant Enterobacterales and nearly 50% for MRSA.
- Antimicrobial consumption in Zimbabwe averaged 32.1 defined daily doses per 1,000 inhabitants per day, with just over 24% of antibiotics falling in the WHO “Watch” category — medicines whose use should be limited to curb resistance.
Zimbabwe launched its second National Action Plan on Antimicrobial Resistance (AMR) (NAP 2.0) for 2024-2028, which uses a "One Health" approach to address AMR in human, animal, and environmental health sectors.
The plan focuses on strengthening surveillance, promoting prevention and infection control, optimising antimicrobial use, building capacity, fostering research, and improving multi-sectoral governance and funding to combat the growing threat of drug-resistant infections.
From Commitments to Action
The 2024 UN General Assembly’s Political Declaration on AMR set ambitious global goals, but experts warn the time for translation into real action is now.
“UN High Level Meeting on AMR 2024 reminded us of immediate action to be taken to safeguard ability to treat humans, animals as well as enhance food security,” said Sjöblom.
As the Jakarta conference continues, participants hope for stronger regional roadmaps that go beyond declarations and bring change where it matters most — in hospitals, farms, communities, and households.

















Leave Comments