Audrey Galawu- Assistant Editor
As the world marks the 30th anniversary of the Beijing Declaration and its Platform for Action, the bold promise made to women and girls in 1995 — to protect their health, dignity, and rights — remains heartbreakingly unfulfilled.
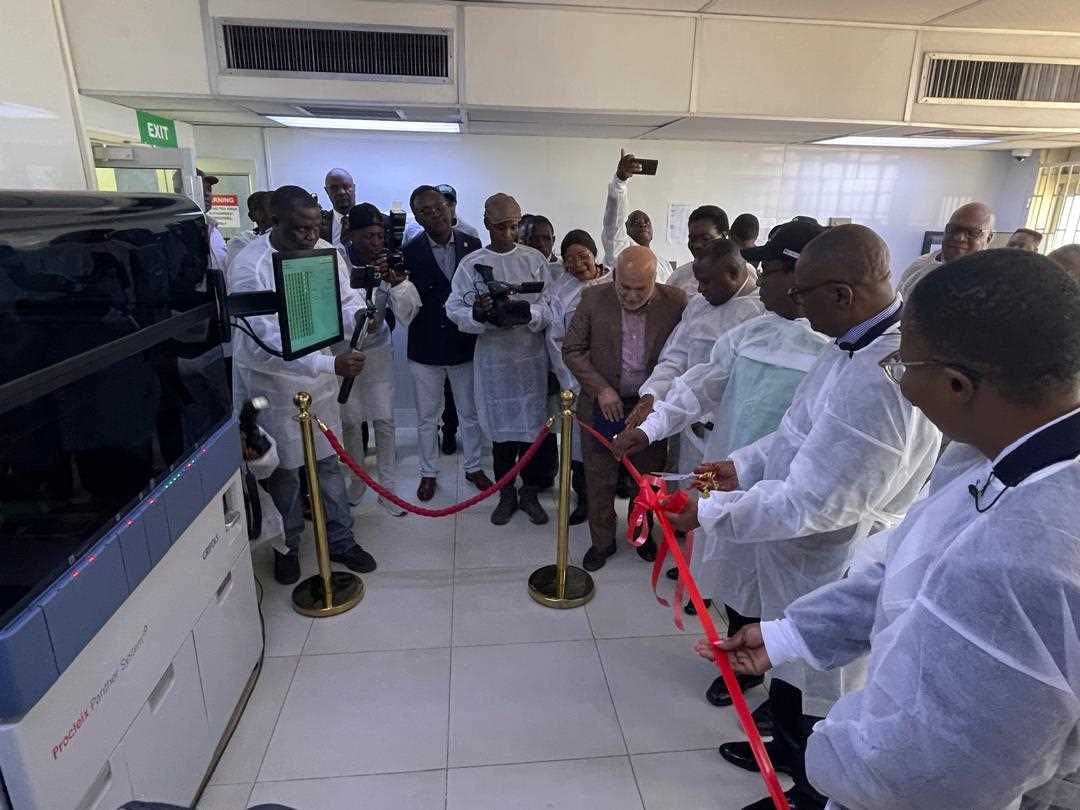
At a critical Side Event held alongside the 78th World Health Assembly (WHA78), global leaders, activists, and survivors gathered to issue a unified call: Universal Health Coverage cannot be universal if it ignores the lived realities of women and gender-diverse people.
“The promise remains unfulfilled,” declared Nazneen Damji of UN Women. “Health systems that ignore women’s unique needs are not only unjust — they are ineffective.”
From escalating funding cuts to rising authoritarianism, speakers painted a sobering picture of a world backsliding on gender equality.
Sexual and reproductive health and rights, long contested, are now under coordinated assault. Damji stressed that only 56% of married women globally have autonomy over their own reproductive health — not just a statistic, she warned, but a reflection of deep-rooted structural injustice.
And the consequences are catastrophic.
- Every two minutes, a woman dies from a preventable pregnancy-related cause.
- In 2023 alone, over 700 women died every day from avoidable complications during pregnancy and childbirth.
- In parts of Sub-Saharan Africa, adolescent girls are over three times more likely to contract HIV than their male counterparts.
“This is a crisis of political will,” Damji said. “SRHR is not optional. It is a fundamental human right.”
The newly released World Report on the Social Determinants of Health Equity underscores what women around the world already know: gender discrimination remains a barrier even when user fees are removed.
For the young, the poor, migrants, and ethnic minorities, abuse and mistreatment often await them in the very places meant to provide care.
“During COVID-19, the most marginalised were pushed even further behind,” said Dr. Harjyot Khosa of IPPF. “Women in all their diversities — LGBTQI+, women who use drugs, sex workers — were left with no access to care.”
Khosa highlighted how health systems are still designed for the “heterosexual, married couple,” ignoring the vast spectrum of real-world identities and needs. “SRHRJ [sexual and reproductive health, rights and justice] must be our first step toward inclusive UHC,” she said.
In the Dominican Republic, skin colour and nationality remain deadly barriers.
“One of my Haitian patients with cervical cancer was denied care due to language,” said Dr. Eliezer Lappots-Abreu of Health Horizons International. “We provided a translator. Still, they refused to treat her because she lacked documentation. Her only options? Palliative care or to die at home.”
These stories, he said, aren’t rare — they are the norm.
Related Stories
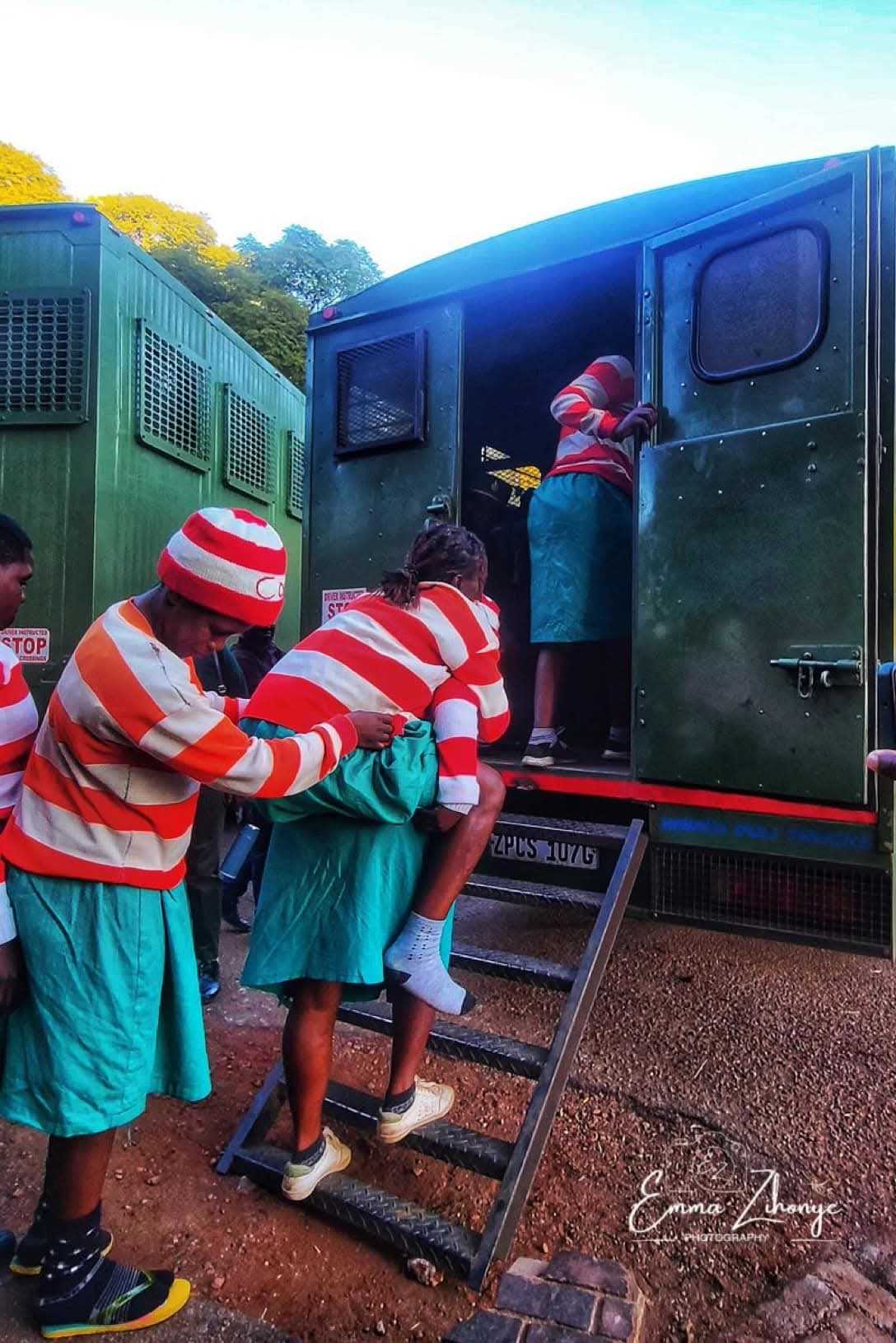
“Survivors of gender-based violence often can’t access healthcare,” said Fadekemi Akinfaderin of Fos Feminista. “Not due to lack of will, but because the healthcare system itself is a site of discrimination — or worse, violence.”
Even the privileged aren’t immune. Akinfaderin, an educated middle-class woman, was denied an epidural during childbirth. “The nurse told me to give birth like a ‘Hebrew woman.’ I don’t even look Hebrew.”
This, she said, is why legal and health systems must work hand in hand to ensure dignity and safety for all.
Baba Aye of Public Services International reminded participants that the "C" in UHC has been misinterpreted as "coverage," when it should mean "care."
Aye pointed out how increasing privatisation under UHC language risks sidelining poor and marginalised groups.
“When 13% of maternal deaths are from unsafe abortions, and most healthcare workers are women themselves, criminalising abortion is not just a health issue — it’s a workforce crisis,” Aye warned.
Health systems cannot be reformed without acknowledging the multi-layered challenges faced by marginalised women.
Maya Ranavare of India’s leprosy survivor network APAL explained how stigma and gender bias intersect to silence women with leprosy, making them unable to seek treatment or express suffering even within their families.
Daxa Patel, an HIV advocate in India, emphasised the toll of out-of-pocket health expenses. “Women with HIV face intersectional stigma — from the system, the community, and within their own homes,” she said.
Nowhere are these challenges more acute than in conflict and authoritarian settings.
In South Sudan, Rachel Adau of the Women’s Empowerment Centre said rape and sexual violence are rampant in conflict zones. “Displacement, disability, and HIV all worsen access to justice and care. The trauma is layered and ongoing.”
UHC must be rooted in justice, equality, and care — not just coverage. It must include everyone, especially those historically excluded.
As Dr. Tlaleng Mofokeng, UN Special Rapporteur on the Right to Health, declared: “Health systems cannot be transformed without a rights-based, gender-responsive approach. UHC must mean dignity for all — not just survival.”
On this 30th anniversary of the Beijing Declaration, the call is clear: Our health systems must stop failing women and gender-diverse people. The time to act is not tomorrow — it is now.

















Leave Comments